Cataract surgery has come a long way in recent years, thanks to the advancements in medical technology. With the introduction of advanced technologies, surgeons are now able to provide better outcomes for their patients. In this article, we will explore the various innovations in cataract surgery and how they are revolutionizing the field.
Understanding Cataract Surgery: A Comprehensive Overview
Before we delve into the advancements, let’s first understand the basics of cataract surgery. Cataract refers to the clouding of the natural lens of the eye, which leads to decreased vision. It is a common condition that affects millions of people worldwide. Cataract surgery is the most effective treatment for cataracts, and it has undergone significant advancements over the years.
Traditionally, cataract surgery involved making a large incision in the cornea and removing the lens manually. This procedure, known as extracapsular cataract extraction (ECCE), required a longer recovery time and often resulted in astigmatism. However, with advancements in technology, the procedure has become less invasive and more precise.
The Evolution of Cataract Surgery
Cataract eye surgery has evolved significantly over the years, thanks to continuous innovation and research. In the past, the only option for cataract treatment was to remove the entire lens, leaving the patient without a natural lens. This approach had its limitations and often required the use of thick glasses or contact lenses to restore vision.
In the 1980s, a major breakthrough occurred with the introduction of phacoemulsification. This technique involves breaking the lens into smaller pieces using ultrasound energy, making it easier to remove through a smaller incision. Phacoemulsification revolutionized cataract surgery, allowing for faster healing, reduced complications, and improved visual outcomes.
Since then, several advancements have been made in cataract surgery, leading to the introduction of advanced technologies that we will explore in the following sections.
The Basics of Cataract Surgery
Before we delve into the advanced technologies, let’s take a closer look at the basics of cataract surgery. The procedure is typically performed under local anesthesia, ensuring that the patient remains comfortable throughout the surgery. The surgeon makes a small incision in the cornea, which is the clear front surface of the eye.
Through this incision, a tiny probe is inserted to break up the cloudy lens. This probe uses ultrasound waves or laser energy to emulsify the cataract, transforming it into tiny fragments. The fragmented lens material is then suctioned out of the eye using a small tube, leaving the clear back portion of the lens capsule intact.
Once the lens is removed, the surgeon inserts an artificial intraocular lens (IOL) into the empty lens capsule. The IOL serves as a replacement for the natural lens, restoring clear vision. There are various types of IOLs available, including monofocal, multifocal, and toric lenses, each offering unique benefits depending on the patient’s visual needs.
The incision made during cataract surgery is typically self-sealing and does not require stitches. This allows for faster healing and reduces the risk of infection. After the surgery, patients are usually given eye drops to prevent inflammation and promote healing.

With the introduction of advanced technologies, such as femtosecond laser-assisted cataract surgery and intraoperative aberrometry, surgeons are now able to perform cataract surgery with even greater precision and accuracy. These technologies allow for customized treatment plans tailored to each patient’s unique eye characteristics, resulting in enhanced visual outcomes.
In conclusion, cataract surgery has come a long way since its inception. From the traditional extracapsular cataract extraction to the modern phacoemulsification technique, advancements in technology have revolutionized the field. With ongoing research and innovation, cataract surgery will continue to evolve, providing patients with safer, more effective, and personalized treatment options.
Also read: Small Incision Cataract Surgery: What You Need to Know
The Advent of Advanced Technologies in Cataract Surgery
With the advancements in technology, cataract surgery has entered a new era. Surgeons now have access to a wide range of innovative tools and techniques that have the potential to enhance patient outcomes and improve overall surgical experience.
Cataract surgery is the most commonly performed surgical procedure in the world, and its success rate is incredibly high. However, with the advent of advanced technologies, surgeons are now able to take this procedure to new heights.
The Role of Technology in Modern Cataract Surgery
Technology has played a significant role in revolutionizing cataract surgery. With the use of advanced imaging systems, surgeons are able to plan and perform procedures with greater accuracy and precision.
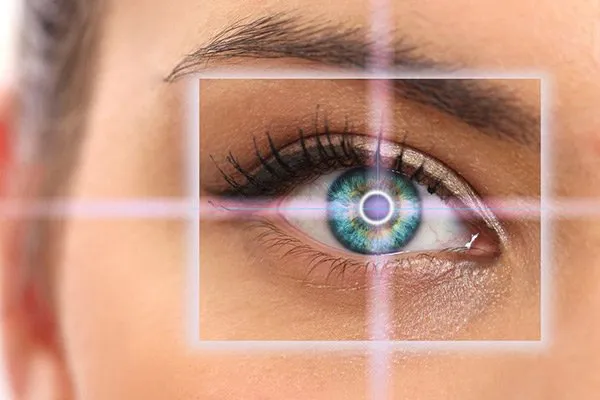
One such technology is the optical coherence tomography (OCT), which allows surgeons to visualize the internal structures of the eye in real-time. This enables them to make more informed decisions during surgery and ensures optimal placement of the intraocular lens (IOL).
In addition to OCT, another groundbreaking technology that has transformed cataract surgery is femtosecond laser-assisted cataract surgery (FLACS). This technology uses a laser to create precise incisions in the cornea, lens, and capsule, resulting in a more predictable and controlled surgical process.
Furthermore, advanced technologies such as phacoemulsification have replaced older techniques, making cataract surgery less invasive and reducing the risk of complications. Phacoemulsification uses ultrasound energy to break up the cloudy lens and remove it through a small incision, allowing for faster healing and better visual outcomes.
The Impact of Advanced Technologies on Patient Outcomes
The introduction of advanced technologies has had a profound impact on patient outcomes in cataract surgery. With improved accuracy and precision, surgeons are able to achieve better visual acuity and refractive outcomes.
Patients who undergo cataract surgery with the assistance of advanced technologies often experience improved visual outcomes compared to traditional methods. The use of OCT and FLACS allows surgeons to precisely measure the eye’s dimensions and customize the procedure accordingly, resulting in better postoperative vision.
Additionally, advanced technologies have also led to faster recovery times and reduced complications. Patients can now experience quicker healing and return to their normal activities sooner. The use of smaller incisions and more precise surgical techniques has minimized the risk of infection and inflammation, leading to a smoother recovery process.
Moreover, the use of advanced technologies has also provided surgeons with more options for customization. This allows for better outcomes for patients with complex cases or specific visual needs. Surgeons can now tailor the procedure to address astigmatism, presbyopia, and other refractive errors, resulting in improved overall vision.
In conclusion, the advent of advanced technologies in cataract surgery has revolutionized the field and improved patient outcomes. With the use of technologies such as OCT, FLACS, and phacoemulsification, surgeons are able to perform procedures with greater precision and achieve better visual outcomes. Patients can now benefit from faster recovery times, reduced complications, and customized treatment options. As technology continues to advance, the future of cataract surgery looks promising, with the potential for even further improvements in patient care and surgical outcomes.
Key Innovations in Cataract Surgery
Now that we have explored the role of technology in cataract surgery, let’s dive into some of the key innovations that have emerged in recent years.
Laser-Assisted Cataract Surgery
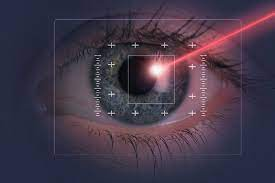
Laser-assisted cataract surgery (LACS) is one of the most significant advancements in the field. This technique utilizes a femtosecond laser to perform various steps of the surgery, such as creating precise incisions and softening the lens for easier removal.
LACS offers several advantages over traditional cataract surgery, including improved incision architecture, reduced energy use, and enhanced safety. It also allows for more precise placement of advanced IOLs.
Micro-Incision Cataract Surgery
Micro-incision cataract surgery (MICS) involves making smaller incisions, typically less than 2.2 mm in size. This technique offers several benefits, including reduced induced astigmatism, faster healing, and improved post-operative vision.
MICS has become increasingly popular due to its minimally invasive nature and quicker recovery times. Surgeons are now able to perform cataract surgery with greater precision and comfort for their patients.
Femtosecond Laser Technology in Cataract Surgery
Femtosecond laser technology has revolutionized the field of cataract surgery. This ultrafast laser allows surgeons to perform various steps of the procedure with unprecedented precision and safety.
With femtosecond laser technology, surgeons can create precise corneal incisions, fragment the lens, and perform astigmatic correction with increased accuracy. This technology has greatly improved the outcomes of cataract surgery and opened up new possibilities for customization.
The Future of Cataract Surgery
As technology continues to advance, the future of cataract surgery holds even more exciting possibilities. Let’s explore some emerging technologies that are set to shape the future of this field.
Emerging Technologies in Cataract Surgery
Researchers and innovators are constantly exploring new technologies to further enhance cataract surgery. One such emerging technology is the use of intraocular robotics. These robotic systems can perform various steps of the surgery with unmatched precision, reducing human error and improving outcomes.
Another emerging technology is the incorporation of artificial intelligence (AI) in cataract surgery. AI algorithms can analyze large amounts of data and assist surgeons in decision-making, increasing the accuracy and efficiency of the procedure.
The Potential of Robotics in Cataract Surgery
Robotic systems have the potential to revolutionize cataract surgery by providing unparalleled precision and control. These robotic-assisted systems can perform tasks such as precise incision creation, lens fragmentation, and IOL placement.
By reducing the reliance on human dexterity, robotics can further improve surgical outcomes and expand the possibilities of customization for each patient.
The Role of Artificial Intelligence in Cataract Surgery
Artificial intelligence has the potential to greatly enhance cataract surgery. AI algorithms can analyze data from pre-operative tests and assist surgeons in selecting the best IOL for each patient.
Additionally, AI can help identify potential complications or adverse events during surgery, allowing for timely interventions and improved patient safety.
Challenges and Considerations in Implementing Advanced Technologies
While advanced technologies offer numerous benefits in cataract surgery, there are also challenges and considerations that need to be addressed.
Cost and Accessibility of Advanced Technologies
One major challenge is the cost and accessibility of advanced technologies. Cutting-edge equipment and systems can come with a high price tag, making them inaccessible to some healthcare facilities and patients.
Efforts are being made to address this issue by providing affordable options and exploring reimbursement options for patients and healthcare systems.
Training and Skill Development for Surgeons
Implementing advanced technologies also requires training and skill development for surgeons. It is essential for surgeons to undergo comprehensive training and gain hands-on experience with these new technologies to ensure optimal outcomes for their patients.
Continuous professional development and ongoing education are crucial in keeping up with the rapidly evolving field of cataract surgery.
Patient Safety and Ethical Considerations
As new technologies are introduced, ensuring patient safety and addressing ethical considerations are of utmost importance. This includes thorough evaluation of the risks and benefits of each technology, as well as clear communication with patients regarding the potential outcomes and limitations.
Ethical considerations also include informed consent, privacy concerns, and equitable access to advanced technologies for all patients.
Conclusion
Innovations in cataract surgery have paved the way for better outcomes and improved quality of life for patients. Advanced technologies, such as laser-assisted cataract surgery, micro-incision cataract surgery, and femtosecond laser technology, have revolutionized the field.
As technology continues to advance, the future of cataract surgery holds tremendous potential, with emerging technologies like robotics and artificial intelligence set to further enhance surgical outcomes.
However, it is important to address challenges such as cost, training, and ethics to ensure that these technologies are accessible, safe, and beneficial for all patients.
With continued research and collaboration between surgeons, engineers, and innovators, the field of cataract surgery is poised for further transformative advancements, ultimately benefiting the millions of people worldwide who suffer from cataract-related vision loss.